Struggling to conceive can feel like an emotional maze. For couples trying to build a family and facing challenges, the good news is that there are several advanced fertility treatments available today that offer real hope.
Hi, I’m Dr. Tolu Binutu — a medical doctor and sexual health content creator. Over the years, my videos have helped millions understand their bodies better and make more informed health decisions. Today, we’re diving into the world of fertility treatments — what’s available, when to consider them, and what to expect.
When Should You See a Fertility Specialist?
Before we talk about the options, let’s clarify who should even be considering fertility treatments:
- Couples under 35 who have been having unprotected sex at least 3 times a week for a year without conceiving.
- Couples over 35, especially women, who have tried consistently for 6 months without success.
- Those who have had:
- Multiple miscarriages
- Irregular or absent periods
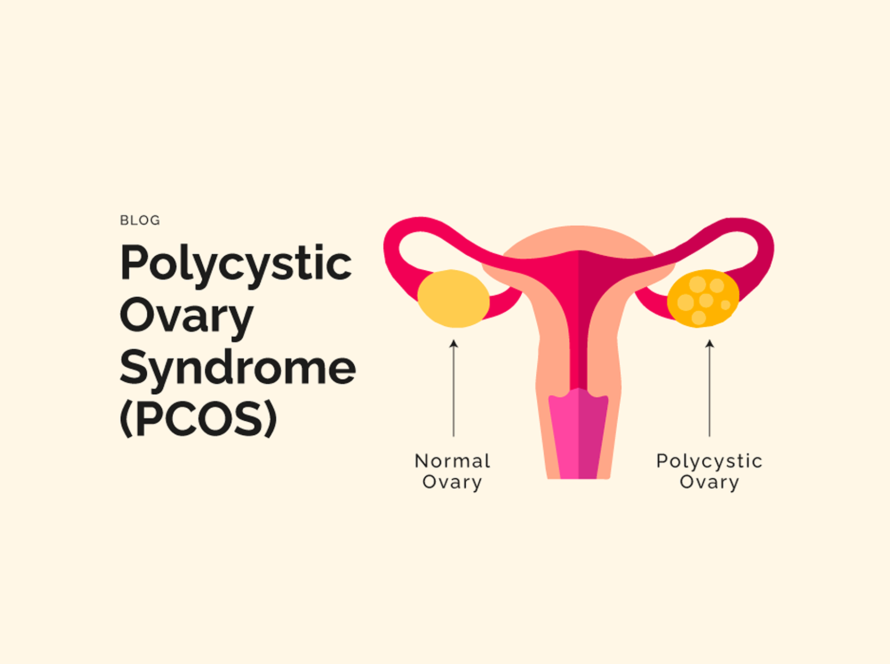
- Known fertility-impacting conditions like fibroids, PCOS, low sperm count, etc.
- Multiple miscarriages
If you fall into any of these categories, it may be time to consult a fertility specialist.
1. Ovulation Induction
This is often the first step in fertility treatment, especially for women who aren’t ovulating regularly (or at all).
How It Works:
- Medications like Clomid (Clomiphene Citrate) or Letrozole are taken early in the menstrual cycle.
- These drugs stimulate the ovaries to produce and release eggs.
Pros:
- Non-invasive
- Less expensive compared to other options
- Can work well for women with PCOS or irregular cycles
Cons:
- Side effects may include mood swings and hot flashes
- Increases the risk of multiple pregnancies (twins, triplets, etc.)
Success Rate:
- Ovulation occurs in 70–90% of women
- Pregnancy rate per cycle: 10–15%
2. In Vitro Fertilization (IVF)
One of the most well-known fertility treatments.
How It Works:
- Eggs are harvested from the ovaries and fertilized with sperm in a lab
- The resulting embryo is then transferred into the uterus
Ideal For:
- Blocked/damaged fallopian tubes
- Ovulation disorders
- Endometriosis
- Male infertility
- Unexplained infertility (when no cause is found in either partner)
Pros:
- Widely used and researched
- Can be tailored for many different fertility challenges
Cons:
- Expensive
- May require multiple attempts before success
Success Rate:
- For women under 35: 55% per cycle
(varies by clinic and individual factors)
3. Intracytoplasmic Sperm Injection (ICSI)
A specialized version of IVF focused on male infertility.
How It Works:
- A single sperm is directly injected into an egg in the lab
Ideal For:
- Low sperm count
- Poor sperm motility
- Previous IVF failures
- Sperm retrieved surgically
Pros:
- Offers hope in cases of severe male infertility
Cons:
- Costly
- May require multiple cycles
Success Rate:
- Fertilization rate: 50–60%, depending on various factors
4. Pre-implantation Genetic Testing (PGT)
Also known as PGD (Pre-implantation Genetic Diagnosis) in some places.
How It Works:
- Embryos are tested for genetic conditions before being implanted
Ideal For:
- Couples with known genetic issues (e.g., AS + AS genotype, sickle cell concerns)
- Recurrent miscarriages
- Women of advanced maternal age
Pros:
- Reduces risk of genetic disorders
- Increases chances of a healthy pregnancy
Cons:
- Very expensive (adds to the cost of IVF)
- Raises ethical concerns around embryo selection
5. Egg and Sperm Donation
For couples who can’t use their own eggs or sperm.
Ideal For:
- Severe male infertility
- Premature ovarian failure
- Certain genetic conditions
Pros:
- Enables couples to still have children despite major fertility barriers
- Relatively high success rate
Cons:
- Ethical and emotional complexities
- Involves a third party, which can be hard to navigate emotionally
Success Rate:
- IVF with donor eggs: 54% success for fresh embryos
6. Gestational Surrogacy
When another woman carries the pregnancy on behalf of the couple.
Ideal For:
- Absence of uterus
- Medical conditions preventing pregnancy
- Recurrent pregnancy loss
Pros:
- Offers a biological connection to the child
- A solid option for those who can’t carry a pregnancy
Cons:
- Very expensive
- Legal contracts and lawyers often required
- Can be emotionally complex, especially involving a third party
Success Rate:
- Surrogacy: 75% success rate
- Once surrogate is pregnant, there is a 95% birth rate
In Conclusion
Advanced fertility treatments offer a lifeline of hope for many facing infertility. Each option comes with its own set of benefits, drawbacks, and emotional considerations. That’s why it’s so important to speak with a fertility specialist — someone who can guide you based on your unique situation and health history. Whether you’re at the start of your fertility journey or exploring new possibilities after years of trying, know this:
You’re not alone, and there are real solutions out there.